Side-effects
Not everyone will get side-effects, as each person reacts differently to the different drugs administered. Some parts of the body, where normal cells grow quickly, are more affected by chemotherapy than others. These are the mouth, skin, hair bone marrow and digestive system.
The effects of chemotherapy on bone marrow
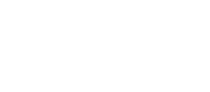
The bone marrow is part of the body where blood cells are made, Red blood cells give you enery, white blood cells fight infections and platelets help the blood clot, to prevent bleeding.
Chemotherapy may slow down the production of these healthy cellsm but this temporary. A blood test, called a Full Blood Count (FBC), is done before each treatment to make sure that you hav enough health blood cells. Quite often, the bone marrow needs more time to recover so your next treatment may need to be postpoined of the dose changed.
What happens if my blood count fails?
White cells: In most cases, your white cells will probably be at their lowest about 7 to 14 days after chemotherapy, so we may ask you for another blood count around this time. This is called an interim or nadir blood count. While your white cell count is low you are more likely to get an infection and could become ill very quickly. It is impoirtant to contact your hospital team if you think you have an infection they can give you antibotics as soon as possible.
Red cells: If you dont have enough red cells, you may get anaemi, which would make you tired and short of breath. SOmetimes, you will need a blood transfusion to help this get better.
Platelets: If the number of platelets in your blood falls, you may start to bruise or bleed more easily. Sometimes you may need a transfusion of platelets to help this.
What are the other common side effects?
Please expand the tabs below which describe the most common side-effects. We will tell you about any side-effects of your treatment. If you notice anything which you think the chemotherapy has caused, but don't find it listed below, please tell one of your hospital team.
Sickness
People react differently to chemotherapy. Some people feel sick after treatment, some people are sick and others have no problem at all.
Some chemotherapy drugs do cause people to feel sick or be sick. If you are being treated with this sort of drug, we will give you antiemetics (drugs which prevent sickness) as part of the treatment. We may prevent sickness as part of the treatment. We may give you some to take home in case you feel sick later.
It is sensible to eat normally before and after treatment, but listen to your body and don't force yourself to eat if you feel sick or are being sick. But it is important to drink at least two to three litres (five pints) of fluid a day.
If you feel sick or are sick after treatment, please tell us because we can change your anti-sickness drugs - there are lots of different types. Other things can help you to feel better for example:
- get enough rest
- change what you eat
- try wearing travel-sickness bands
- hypnotherapy
- relaxation
- simply do things you enjoy
Taste changes and altered appetite
Chemotherapy can make some food taste different. Many people go off tea and coffee and some people get a metallic taste or food cravings. All this might affect your normal diet and make you lose or put on weight. If you get an unpleasant taste in your mouth it may help if you:
- chew celery, fresh pineapple or low-sugar gum
- suck ice lollies
- drink herbal tea or ginger drinks
Your tastes should go back to normal when the treatment has finished.
During your treatment, try to eat a well-balanced diet. Small regular meals will probably make you feel better than if you eat a lot at once. The smell of cooking may make you feel sick during chemotherapy; your food may taste better if someone else cooked it. Some people prefer to cook a few meals at once and freeze them. If you have a problem eating, ask us for advice. We could give you some nutritious drinks or food supplements, or refer you to a dietician.
Sore mouth
It is important that you keep your mouth clean and moist. This helps prevent:
- infection
- problems with your teeth
- mouth ulcers
- fungal infections such as thrush
After cleaning your teeth with a fluoride toothpaste, rinse your mouth well with water to remove debris. Please avoid using commercial mouthwashes. We can give you an antibacterial mouthwash if needed. A soft, child's toothbrush is useful for regular brushing.
If you have false teeth, you should clean them after every meal, and you may be more comfortable without them if this is possible. A lip salve will help to keep lips moist.
Hair loss
Not all chemotherapy drugs cause hair loss. If this does happen, your hair will begin to grow back four to six weeks after your treatment has finished. At first, your new hair may be more curly, thicker or finer, or be a slightly different colour.
Chemotherapy can make your hair brittle and dry, so its a good idea to use a mild or baby shampoo. Do not have your hair set, permed or coloured with products that contain ammonia. Use hair dryers on a cool heat and do not use heated tongs or hot brushes. You can gently brush or comb your hair with a wide-toothed comb every day, but not too often. You may be more comfortable wearing a hairnet or turban at night.
Wigs are available on the NHS, but there may be a prescription charge. It is a good idea to choose a wig while you still have your own hair, so we can match your won style and colour more easily. Your chemotherapy nurse will be able to arrange this fo you. You can wear hats, caps, turbans and scarves to cover thinning hair, and they are usually cooler to wear than a wig.
We may offer you 'scalp cooling' during treatment, which can make hair loss less likely. This only makes a difference with some types of chemotherapy and is only appropriate for some illnesses. We will answer any questions you have about this.
Check here for further information on coping with hair loss.
Fatigue (extreme tiredness)
Most people who are treated with chemotherapy suffer fatigue at some time or another; this is normal. This fatigue can be caused by the chemotherapy or by side effects. The fatigue can be severe, and varies from person to person. Some people can carry on normally, others find that they have to take life more slowly during treatment. You may have to work part time, or give up work temporarily, cut down on social activities and get help with the housework. Gentle exercises can be helpful. You also need to make sure you get enough rest.
There are many thing you can do to reduce your fatigue, and you can discuss these with the nurse who is caring for you.
Sore veins/Phlebitis
Some chemotherapy drugs may cause tenderness or soreness in your arm. Please let your nurse know if you experience any pain or discomfort when you are having your treatment.
Extremely rarely, however, a small amount of the chemotherapy may leak out of the vein into the surrounding tissue. This is know as extravasation. It is important that you let your hospital team know, as soon as possible, if you develop any pain or redness around the area you had your injection at any time after your treatment. Simple procedures can then be followed to reduce any damage.
Reaction to sunlight
Chemotherapy drugs can make you more likely to get sunburnt, both during treatment and for some months after. Use factor 15 (or higher) sun cream or sun block when you are in the sun for any length of time. You can also protect your skin by covering up with loose-fitting clothing, wearing a hat or just trying to stay in the shade. Do not use a sun bed while you are having chemotherapy.
Sex and fertility
Side effects of treatment may mean that your desire for sex is reduced. When your treatment has finished, your energy levels should return to normal.
Women: Often find their periods become irregular or stop during treatment. Some women remain fertile and it is important that you do not become pregnant during chemotherapy, and for at least one year afterwards, because it may damage the developing baby. It is very important that you use contraception, and the best methods at this time are barrier methods such as condoms of the cap. Condoms will also reduce the risk of infection. Check with your hospital team if you are worried about this.
Chemotherapy may make you less fertile. This may be temporary or permanent, depending on your treatment and age. The younger you are, the more likely it is that your periods will go back to normal and you may still be able to get pregnant. If you are close to the menopause, your periods may stop permanently.
If you are planning to become pregnant in the future, you may want to discuss this with your hospital team before your chemotherapy starts.
It is best not to breast-feed while you are having chemotherapy because the drugs may be passed on to the baby. If you are worried, please discuss this with your hospital team.
Your vagina may become more dry because of chemotherapy. This can make sex difficult or painful. Using a lubricant, like K.Y Jelly or Replens, inside the vagina before sex should make it easier.
Men: Some chemotherapy drugs can reduce fertility. If this is likely, we may discussed storing your sperm with you before treatment. We will store your sperm before your treatment begins. You may remain fertile during the early part of your treatment. It is important that you do not father any children during treatment, and for one year afterwards, because your sperm may not be formed properly which could damage the developing baby.
You or your partner should use effective contraception, you can discuss this with your hospital team.
Mood changes
You may notice a change in your moods, such as becoming more anxious or easily upset by things. Many people find themselves worrying about whether or not the treatment is working.
These feelings are normal during chemotherapy, and may be harder to cope with because you are feel tired and your normal routine has changed. Talking about your moods and feelings with close family or friends can be very helpful for you (and them!)
Sometimes, it is useful to talk to other patients who have had a similar treatment to yourself. Nurses, psychologists and counsellors will also support you. Your hospital staff will be able to tell you about this.